Navigate Fertility Add-Ons: Advocate for Yourself and Choose What Works for Your Journey
Sep 29, 2025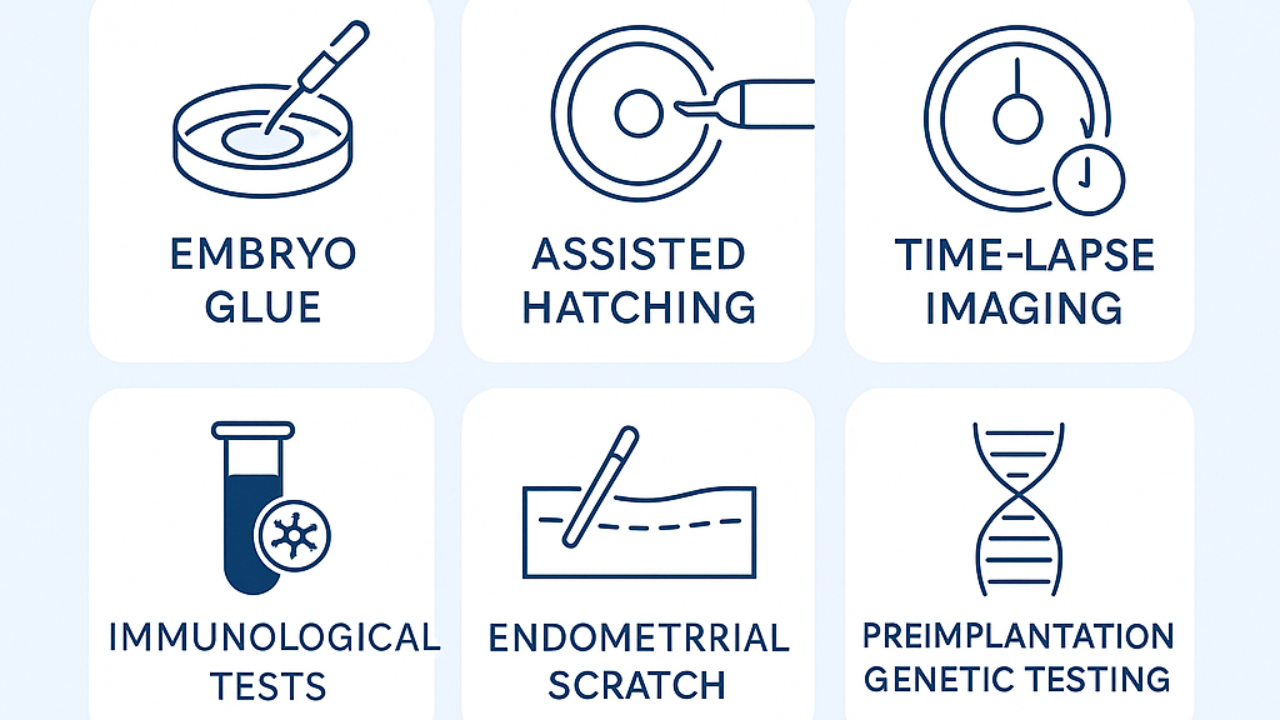
In the fertility landscape, add-ons like preimplantation genetic testing (PGT), endometrial scratching, or time-lapse imaging are often presented as ways to boost success rates. But the Human Fertilisation and Embryology Authority (HFEA), the UK's authority on reproductive medicine, has been ramping up criticism of these, highlighting in their September 2025 draft guidelines that many lack robust evidence and can give false hope while driving up costs. As a Fertility Doctor with over a decade of experience, I've heard from countless women who feel immense pressure to opt for these add-ons, fearing they'll miss out on optimal chances without "trying everything." This pressure often stems from clinic marketing that positions them as must-haves, yet a UK survey shows 73% of IVF patients pay for them despite limited benefits.
The real issue? Without personalized explanations, women can't discern which add-on might truly fit their case. The HFEA's stance urges better transparency, but at the end it often falls on patients to advocate. Some add-ons can make sense in specific scenarios, while others may be unnecessary, adding costs (up to $1,000+ per treatment) without proportional gains. The solution lies in education: Understanding the evidence empowers you to make informed decisions, potentially saving money and avoiding emotional burnout.
Let's break down some common IVF add-ons, their potential benefits, and the evidence behind them (based on HFEA ratings and recent reviews like the Italian SIFES-MR 2025 and ESHRE guidance on 28 add-ons). I'll focus on personalization, when it might be worth considering for your unique situation.
- Preimplantation Genetic Testing (PGT): This screens embryos for genetic abnormalities before transfer. Potential benefits include reducing miscarriage risk in cases with known genetic issues or advanced maternal age, potentially improving live birth rates by 10-20% in select groups. Evidence level: Moderate (HFEA green in some cases, but red for routine use in low-risk patients). When it makes sense: For women over 35 with history of chromosomal issues or recurrent losses. Cost: $3,000–$5,000. Twist: If you're low-risk, skipping could save money, advocate by asking for your euploidy rates first.
- Endometrial Scratching: A procedure scratching the uterine lining to potentially improve implantation. Potential benefits: Some studies suggest a 5-10% boost in implantation for women with repeated failures. Evidence level: Limited (HFEA red; criticized for inconsistent results). When it makes sense: Possibly for recurrent implantation failure, but only after ruling out other factors. Cost: $200–$500. Twist: Pressure often leads to unnecessary use, educate yourself on alternatives like progesterone testing to avoid it if not needed.
- Time-Lapse Imaging (e.g., EmbryoScope): Monitors embryo development continuously without disturbing them. Potential benefits: May improve embryo selection, with some data showing 5-15% higher success in certain clinics. Evidence level: Limited (HFEA amber; not proven superior to standard incubation). When it makes sense: For patients with poor embryo quality or multiple cycles. Cost: $500–$1,000. Twist: If your clinic's standard monitoring is solid, this might be overkill, ask for comparative data to decide.
- EmbryoGlue: A hyaluronan-rich medium to aid embryo attachment. Potential benefits: Small studies indicate a 5-8% implantation boost in some cases. Evidence level: Limited (HFEA red; mixed results). When it makes sense: Possibly for older embryos or sticky implantation issues. Cost: $100–$300. Twist: Often added routinely, educate on evidence to skip if your case doesn't warrant it, saving unnecessary expense but fairly low costs compare to benefits.
- Assisted Hatching: Thinning the embryo's outer shell to help implantation. Potential benefits: Can increase success by 10-15% in women over 38 or with thick zona pellucida. Evidence level: Moderate (HFEA green in select cases, red for routine). When it makes sense: For frozen cycles or poor embryo quality. Cost: $300–$600. Twist: Pressure leads to overuse, advocate by requesting embryo grading reports first and ask for the recommendation of the Embryologist.
- Immune Therapies (e.g., Intralipids): Infusions to suppress immune responses. Potential benefits: May help with implantation in autoimmune-related failures, with anecdotal 10-20% improvements. Evidence level: Very limited (HFEA red; risks like infections outweigh unproven gains). When it makes sense: Only for confirmed immune issues after testing. Cost: $500–$1,500. Twist: Often sold as a catch-all, insist on immune panels to avoid wasting money.
The twist? Being informed and educated flips the script from pressure to power. Instead of feeling compelled to "try everything," focus on evidence-based choices tailored to your case. This not only boosts confidence but can save thousands, avoiding add-ons unless they fit your profile. ESHRE and SIFES-MR guidelines echo this: Personalization is key. In my coaching, we dive into your data, weigh options, and craft a plan that prioritizes what matters most to you—saving time, money, and heartache.
If add-ons have left you confused, know empowerment starts with knowledge. Book a free 15-minute Clarity Call at eggcellentfertility.com to personalize your path. Let's ensure your journey is informed, not overwhelming.
Book a Free Eggcellent Clarity Call with me and we figure out your TTC Strategie!
Stay connected with news and updates and get my Guide The Eggcellent Fix to change your journey!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
